Iron Deficiency in Women: Can You Be Iron Deficient Without Anemia?
Written by TYE Medical on Feb 21st 2024
You need iron to produce and maintain healthy red blood cells. When you lack enough iron you’re at risk for developing anemia. But what you may not realize is that you can have low iron levels without being diagnosed as anemic. It’s true that iron deficiency is the most common cause of anemia, which is why doctors might rule out an iron problem if you test negative.
If you have anemia, your red blood cell count is too low, commonly causing fatigue and weakness. About 20% of the worldwide population has iron-deficiency anemia, making it one of the most common nutritional deficiencies in the world. Your body needs iron to make enough healthy red blood cells.
But three times as many people have low iron levels with a healthy amount of red blood cells. And doctors might not look any further or discover you are low in iron. If left undiagnosed and untreated, iron-deficiency can progress until your red blood cells diminish and you become anemic.
Let’s take a closer look at the symptoms and signs of iron deficiency without anemia and how it’s treated.
Symptoms of Iron Deficiency Without Anemia

So the diagnosis is different but are the symptoms the same? Will you suffer the same side effects as a person with diagnosed anemia? In some ways, yes. Both conditions share the most common symptoms, such as:
- Fatigue and lethargy
- Trouble focusing and concentrating
- Mood changes
- Weakness while active
Anytime you notice these symptoms, it’s worthwhile to check with your doctor. Women should have their iron levels checked at least occasionally since women are very prone to iron-deficiency due to menstruation and childbirth. Your doctor can order blood tests to learn more about your iron and red blood cell count.
Think of iron deficiency as a factory that falls behind production demands. It might take weeks for it to fall below the minimum productivity mark, and once it does, it’s tough to catch back up. It’s the same with our iron stores. If we experience several different factors that are draining our iron stores, we’ll use them up more quickly and be less equipped to rebuild them.
What Causes Iron Deficiency?
You may find one cause of low iron or three. Sometimes it’s a combination of factors. But the most common causes include:
- Not getting enough iron through food or supplements
- Needing more iron than usual (heavy bleeding, surgery, childbirth, etc.)
- Poor iron absorption
You’re more likely to develop iron deficiency if you:
- Are a vegetarian or vegan (meat, especially red meat, is iron-rich)
- Are pregnant
- Are still growing (children and teens)
- Are an athlete
- Have active celiac disease or inflammatory bowel disease
- Have had gastric bypass surgery
- Experienced changes in stomach acid from H. pylori infection or from using proton pump inhibitors (a class of medication that treat acid reflux)
- Are of childbearing age, especially if your periods are heavy
- Have lost blood due to surgery or internal bleeding
What Do Ferritin and Hemoglobin Have to Do with Iron Deficiency?
Ferritin plays a critical role in iron deficiency, because it's a protein that stores and releases iron when needed. When you’re running low on iron, your body pulls it from your ferritin reserves, and if not replenished, these stores can become depleted. This means that you can have low ferritin and temporarily have normal iron levels.
According to the World Health Organization (WHO) low iron is equivalent to ferritin under 12 mcg/L. But other studies suggest you could be considered iron deficient with ferritin levels under 30 mcg/L. Blood tests are available to determine to ferritin levels and blood saturation.
Hemoglobin can be impacted when your iron levels drop low enough for long enough. It’s the part of your red blood cells that carry oxygen. But you need iron to make healthy red blood cells and hemoglobin. So the less iron in your bloodstream, the less hemoglobin, and the less oxygen your cells receive. This is what triggers that list of symptoms, including fatigue.
What Is Anemia?
You're diagnosed with anemia if your ferritin and hemoglobin (and red blood cells) are both low. This is considered iron-deficiency anemia and is very common. But if your hemoglobin is unaffected even though your ferritin is normal, it’s considered iron deficiency without anemia. However, if your ferritin levels don’t improve, it’s likely to progress to anemia as you’re unable to produce enough iron to make red blood cells and hemoglobin.
Blood tests to diagnose anemia usually include ferritin and hemoglobin. Your doctor and run other tests to learn more about your red blood cells and how healthy they are. This can provide a more detailed picture of what is going on in your body.
How Much Iron Do You Need?
Women who menstruate require 18 mg of iron each day to maintain health. You may need more if you’re pregnant or nursing. If you're postmenopausal you need 8 mg daily.
You can get iron from several food sources, but the most easily absorbed iron comes from red meats. However, you can get plant-based iron from leafy green vegetables, beans, lentils, and iron-fortified breakfast cereals.
How Do You Treat Iron Deficiency without Anemia?

Your doctor will first consider your diet and recommend that you adjust your diet to include quality sources of iron. But if you have problems absorbing iron, this won’t be enough. Often supplements are also advised.
In more severe cases, your doctor might recommend iron infusions. When you receive iron infusions, you receive iron through an IV (intravenously). This is done over several visits. It gets iron into your system in greater quantities and more quickly.
After treatment, whether through infusion or supplements, you’ll likely have follow up visits to see how the treatment is working and if there are any changes in your blood test results.
How Much Iron Should You Take?
You should have doctor supervision while taking iron supplements. Taking iron when your levels are within normal range can be dangerous. Elevated iron levels can also cause serious health problems.
Your doctor will likely prescribe a supplement that delivers 28-50 mg of iron. The average supplement provides 15 mg of iron per serving.
Iron Deficiency and Celiac Disease
According to the American Gastroenterological Association recommendations, anyone with unexplained iron deficiency should be tested for celiac disease.
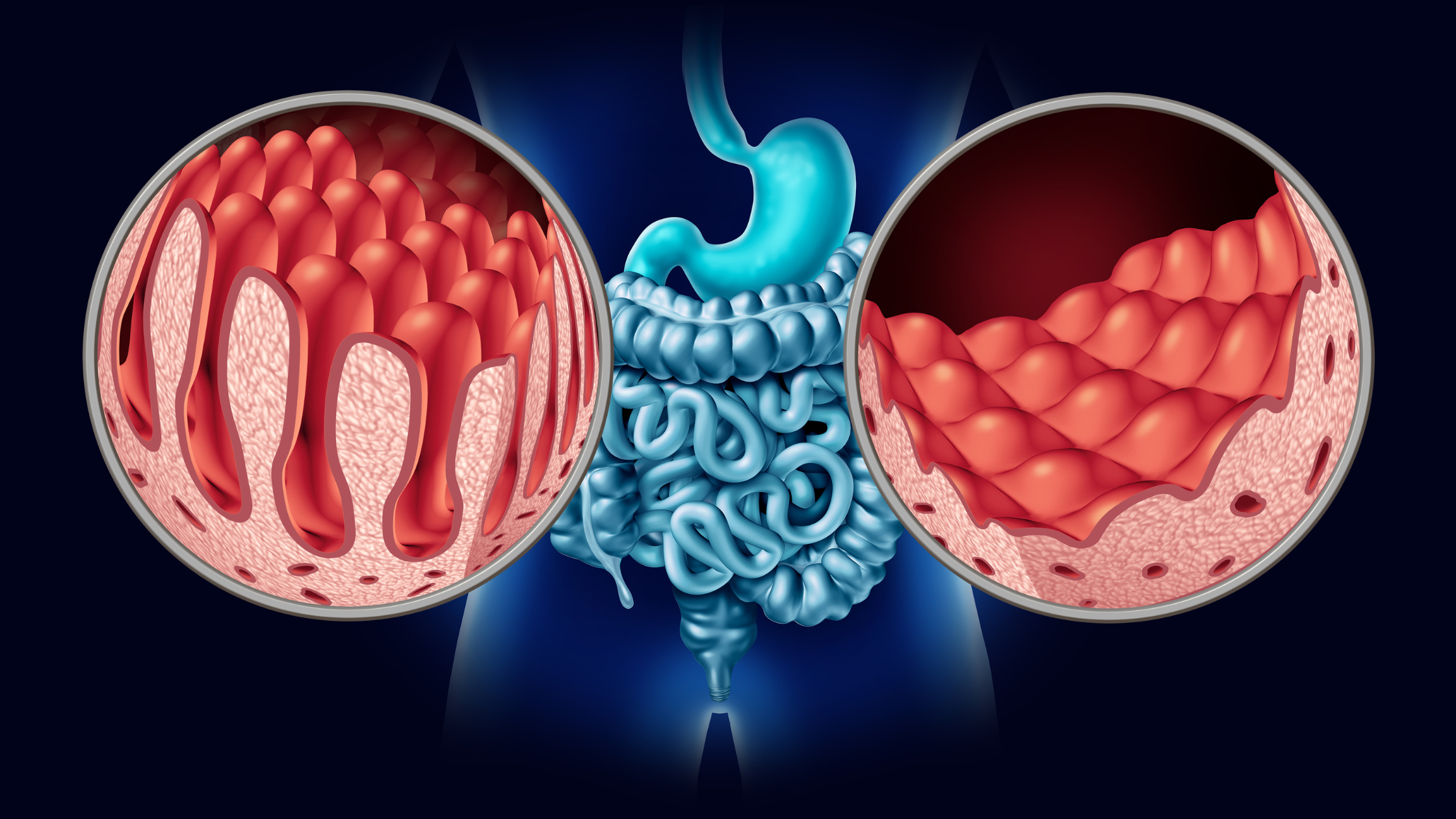
If you have celiac disease, a protein found primarily in wheat sets off an autoimmune response causing your immune system to attack your small intestines. The resulting damage makes it difficult to or impossible to absorb the nutrients from food your body needs. The small intestines are where most nutrient absorption happens.
Other Celiac Symptoms
For some people, iron deficiency, or even anemia, is the primary symptom of celiac disease.
You might have few, if any, gastrointestinal symptoms.
Additional celiac symptoms include:
- Diarrhea
- Constipation
- Abdominal pain
- Nausea/vomiting
- Lactose intolerance
- Unexplained weight loss or gain
- Fatigue
- Memory problems
- Bone or joint pain/arthritis
- Bone loss
- Skin rashes
- Mouth ulcers
- Headaches
- Irregular menstrual cycle
This is just a short list of possible celiac symptoms, and remember that you might not have any symptoms at all other than low iron levels. It’s also possible to have only non-digestive symptoms. Or, the digestive symptoms could be so subtle that you don’t connect them to a possible celiac problem.
Some evidence suggests that if your main digestive system is iron deficiency but with no digestive symptoms, your celiac disease may be more severe than those with additional symptoms.
But once you have been on a gluten-free diet for a while, your small intestines can begin to heal. Your symptoms should also decrease.
Treating Iron Deficiency When You Have Celiac Disease

If you have celiac disease, increasing dietary iron may not benefit you much. If your small intestines haven’t healed, you won’t be able to absorb much or any of the iron from food. It’s still important to eat a healthy, well-balanced diet. This will allow you to gain the nutrition that you can while also helping you avoid other consequences of an unhealthy diet.
If you have celiac disease, you’ll need to rely more on supplements, and especially those that are easier to digest.
Maintaining Healthy Iron Levels to Prevent Deficiency

Detecting low iron levels is the first step. Oftentimes, iron deficiency goes undetected until symptoms worsen. If you have unexplained fatigue, hair loss, difficulty concentrating, mood swings, and weakness during activity, you should see your doctor to rule out low iron levels.
Be sure to eat a healthy, iron-rich diet and take iron supplements as your doctor prescribes. If your doctor hasn’t been able to determine an obvious cause for your iron deficiency, you should test for celiac disease. Typically a blood test is first and, if warranted, is followed by an endoscopy to confirm small intestine damage.
A gluten-free diet will eventually allow your small intestines to heal and perhaps begin absorbing iron properly again. But until then, you’ll need to continue taking an iron supplement.